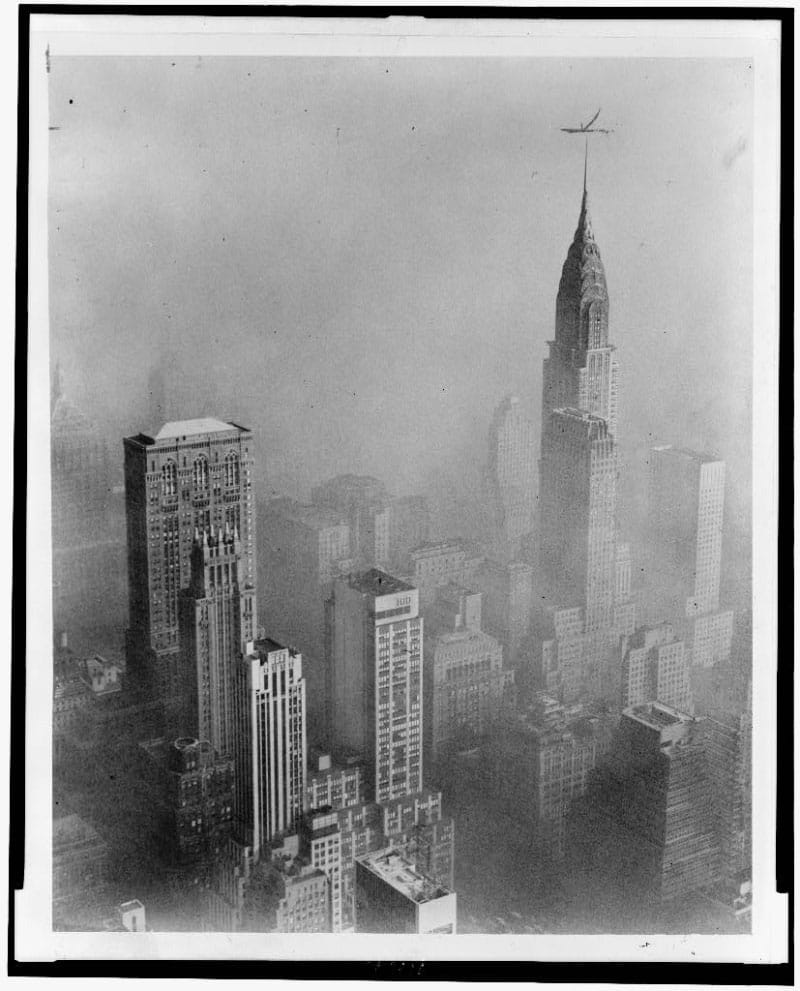
For a quick summary of the fight for clean air over the past century, look out of any office window.
Odds are your view won’t be obscured by dangerous smog – or by clouds of cigarette smoke. For much of the past century, that would have been unthinkable.
“Even since just the 1980s, air pollution has fallen dramatically,” said Dr. Robert Brook, a professor of cardiovascular medicine at Wayne State University in Detroit. He can see the improvement just by watching the background when movies from that era come on. “It’s amazing, the change. And it happened slowly enough that people don’t notice it.”
The change came because of an interaction among scientists, the public and their government that continues to this day, he and other experts say. The science involves particles with complex names and massive amounts of data, but the stakes could not be simpler.
Many people have heard, “You are what you eat,” said Brook, who has been studying air pollution since the 1990s. His version is, “You are what you breathe.”
Discussions about smoking and air pollution often focus on cancer, asthma and other lung diseases. But what we inhale has a big effect on heart and brain health, too.
We now know that even a few cigarettes a day or exposure to secondhand smoke can sharply increase the risk of heart disease and stroke. Air pollution, meanwhile, is associated with an increased risk of heart attack, stroke and death from cardiovascular disease.
The story of how science came to understand that doesn’t begin in the 20th century, said Dr. Sanjay Rajagopalan, chief of cardiovascular medicine and chief academic and scientific officer at the University Hospitals Harrington Heart and Vascular Institute in Cleveland. He’s also a professor of medicine and biomedical engineering at Case Western Reserve University.
Rajagopalan, who worked with Brook on some of the first articles about air pollution and heart disease, said that dirty air has been an issue “ever since man discovered fire.”
The U.S. chapter of that story might begin with cigarettes.
Tobacco – which contains the highly addictive substance nicotine and other harmful chemicals – had been grown in the Americas for thousands of years, but as described in Allan M. Brandt’s 2007 “The Cigarette Century,” a combination of technology, business maneuvers, marketing and shifting social norms turned the U.S. into a nation of smokers. In 1900, American adults smoked an average of 54 cigarettes per person per year. By 1963, that number peaked at an estimated 4,345, according to a 2007 report from what is now the National Academy of Medicine.
With that came an alarming rise in lung cancer, which spurred innovations in how medical research is done.
Some of the earliest studies on smoking were done in Great Britain by Dr. Richard Doll and Dr. Austin Bradford Hill. Their initial work, in 1950, compared 709 people with lung cancer with an equal number of people without cancer. They followed that with a landmark survey of 40,000 doctors. The results, published in 1956, showed that deaths from lung cancer and heart disease were related to how much someone smoked.
By 1960, the American Heart Association was ready to say, “the data strongly suggest that heavy cigarette smoking may contribute to or accelerate the development of coronary heart disease or its complications.”
The tobacco industry worked mightily to sow confusion, so researchers had to build an ironclad case to explain the risks. The U.S. surgeon general’s 1964 report on smoking and health did just that. Not only did it declare that smoking was a cause of cancer, but it also helped establish the modern framework for using data from epidemiological surveys to make connections that couldn’t come from simply studying cells under a microscope.
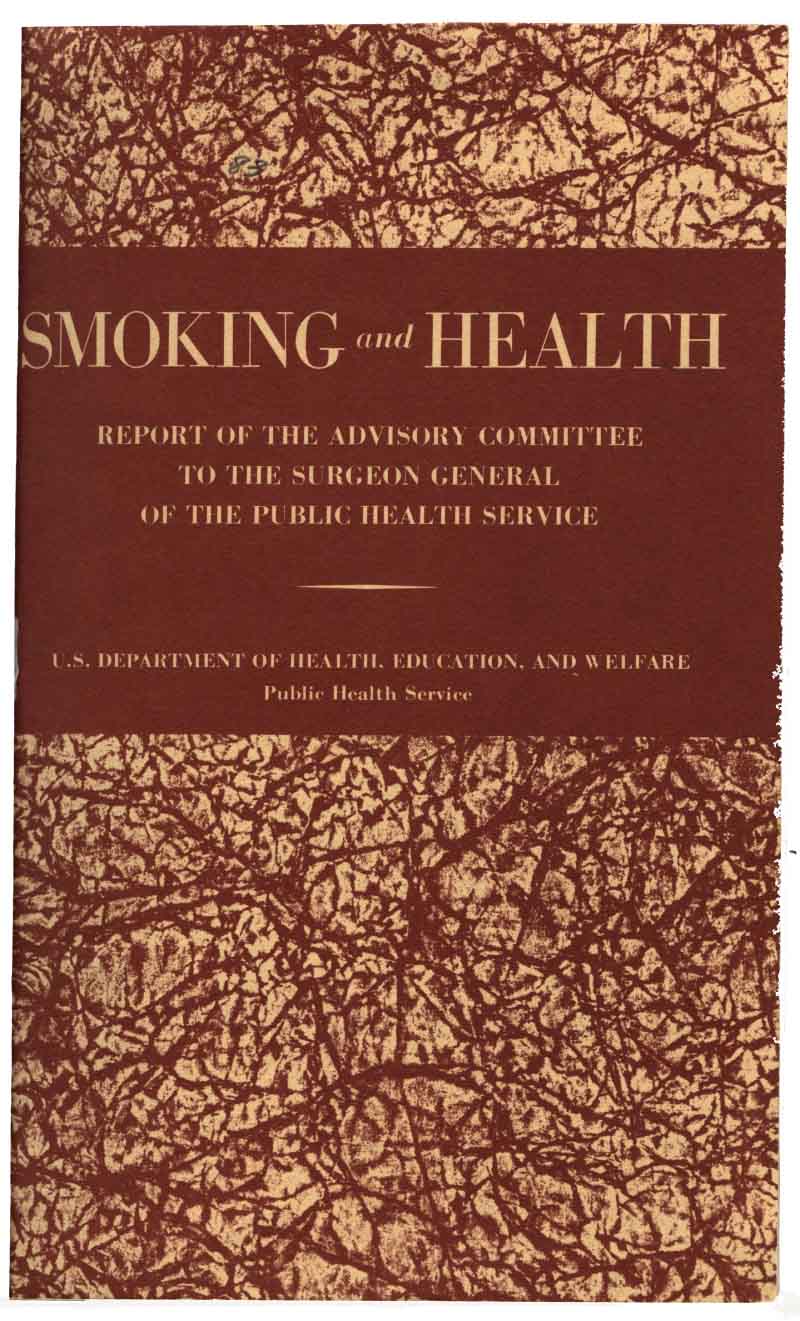
The battle between health advocates and tobacco companies was hardly settled then, but it was a turning point. In 1965, nearly 42% of U.S. adults – including Surgeon General Dr. Luther Terry – were smokers. By 2021, according to the latest Centers for Disease Control and Prevention data, only 11.5% were.
A pattern of crisis leading to change also unfolded with air pollution.
In 1948, a deadly smog formed in Donora, Pennsylvania, killing at least 20 people and sickening thousands. Four years later, the “Great Smog of London” killed as many as 12,000 people.
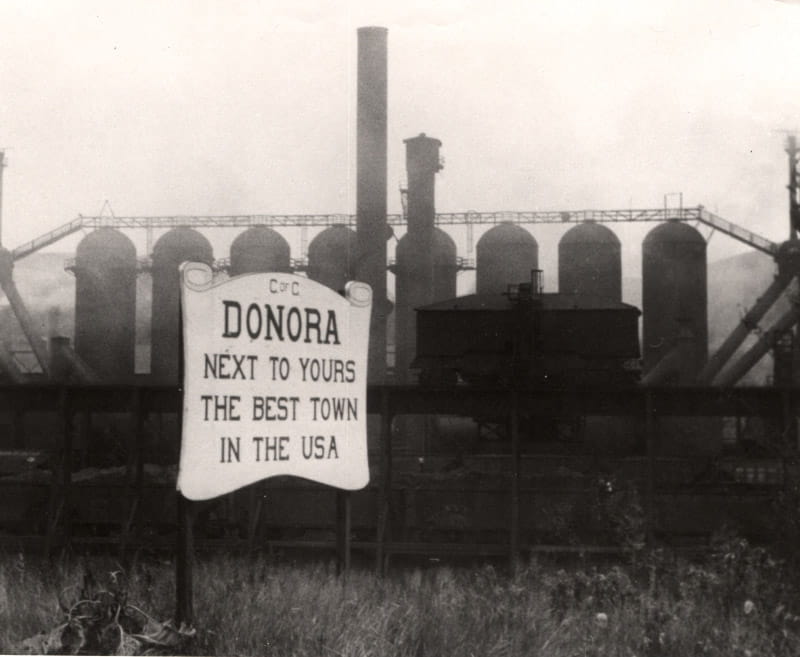
Those and other events helped drive passage of the Clean Air Act of 1970 in the U.S., which Rajagopalan credited for a “massive” improvement in air quality. Since that law took effect, levels of regulated pollutants have dropped 78%, according to the Environmental Protection Agency.
The pattern would repeat itself with secondhand smoke. The first large studies on its dangers appeared in the early 1980s. By 1990, smoking was banned on most U.S. flights. In the following years, many states would pass laws requiring smoke-free workplaces and public places, including bars and restaurants.
Dr. Stacey Alexeeff, a research scientist and biostatistician at the Kaiser Permanente Northern California Division of Research, said that scientists, the public and regulators affected one another. After public outcry led to the Clean Air Act, the regulations required monitoring to measure pollution, which provided more data about health effects. The findings led to changes in regulations to protect health.
Brook said his own work followed such a path. In the mid-1990s, he was launching his career just as some of the first work linking air pollution with cardiovascular disease was being done. Legal challenges to new pollution standards led to the need for more research. In 2004, he was able to lead an expert panel in writing an AHA scientific statement that saw “a strong case that air pollution increases the risk of cardiovascular disease” but also that more research was needed.
By 2010, he led another AHA panel, this one including Rajagopalan, that was able to declare that microscopic particles of pollutants known as PM 2.5, or soot, could cause cardiovascular disease and death. In February of this year, the EPA announced tighter limits on such pollutants, the main sources of which are diesel and car exhaust and coal-fired power plants.
Many things about science and research changed radically over the past century. Thanks to technology, the cycle of science and policy is speeding up, Rajagopalan said. “In every sphere of medicine and public health, the feedback loops are getting faster.”
Alexeeff said that researchers today are emphasizing connections between clean air and socioeconomic status. “The question of how do we protect the most vulnerable populations is a really important one,” she said.
But some current issues are the same as the old. Problems from cigarettes didn’t show up until years after masses began using them. Today, the advent of vaping is exposing people to chemicals whose effects are only beginning to be understood.
And just as in the days of the original Clean Air Act and the first studies on smoking, talk of regulation turns air into a political issue. “I’m not a politician,” Rajagopalan said, but it’s a simple fact that elected officials can alter the future of clean air.

For researchers, the biggest issue in that future is climate change.
Rajagopalan has written that higher temperatures boost ozone levels while also increasing risks of wildfires and dust storms, which produce pollutants that hurt heart health. Researchers also will need to identify the best ways to protect people from such problems – whether it’s masks, air filters or something else, Brook said.
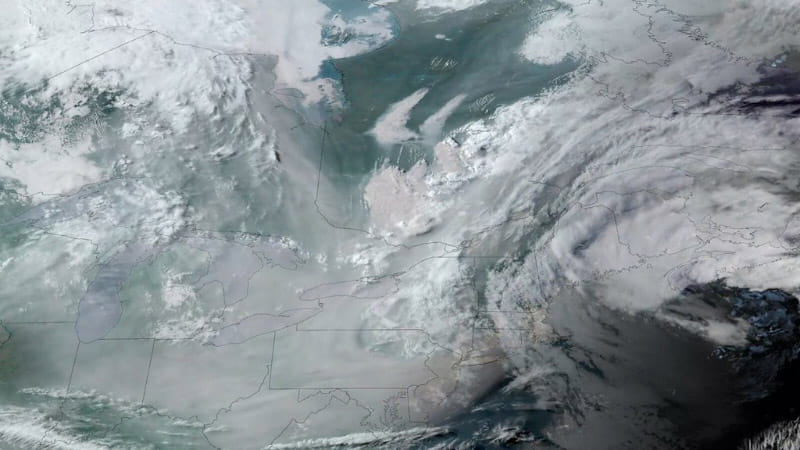
He recalls how last summer, smoke from Canadian wildfires unexpectedly blanketed Detroit and other portions of the Midwest and East Coast, giving them some of the worst air pollution in the world. Brook drew parallels to the “massive public health catastrophes” of London and Donora that reshaped public opinion.
That’s what will shape the future, he said. “Nothing’s going to happen if the public doesn’t demand it.”
Brook said he wished people were more aware of just how much their health depended on clean air – and how much better things had gotten.
“Science informs; the bureaucrats can make decisions,” he said. “We need to be aware of how much benefit has occurred during just our lifetimes, and how important this is for ourselves.”