With the release of new guidelines for treating and managing cholesterol, you may have some questions – not only about the changes in the update, but about cholesterol itself.
Let’s start by acknowledging that while cholesterol is often talked about, it’s tricky to understand.
You probably know that high cholesterol is bad. However, you may not know there’s a bigger picture involved when determining what’s considered too high. Put another way, the same number could be in the normal range for you but considered high for your best friend.
The only way to know your cholesterol situation and, more importantly, what to do about it, is by working with your health care provider. If a healthier lifestyle and/or treatment is needed, your provider will work with you to determine the best plan. This is important because poorly managed cholesterol could lead to heart attack, stroke and other major health problems.
Below is essentially a brief Cholesterol Care 101 course, the basics needed to understand, treat and manage cholesterol. Answers are based on years of established science with added insights from cholesterol experts.
What is cholesterol?
“First of all, it’s important for people to understand that cholesterol is itself not a bad thing,” said Dr. Robert Eckel, former president of the American Heart Association. “Cholesterol is an important part of the body that every cell has on its surface. But in our bloodstream, we don’t want too much and the vehicle that carries it can be important.”
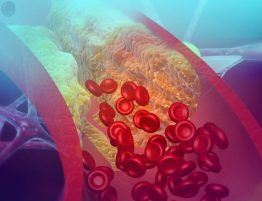
Cholesterol is a waxy substance your body uses to build cells. Your liver makes all the cholesterol you need. However, dietary cholesterol – the kind you take in through food and some drinks (like milk) – causes your liver to send even more cholesterol into your bloodstream.
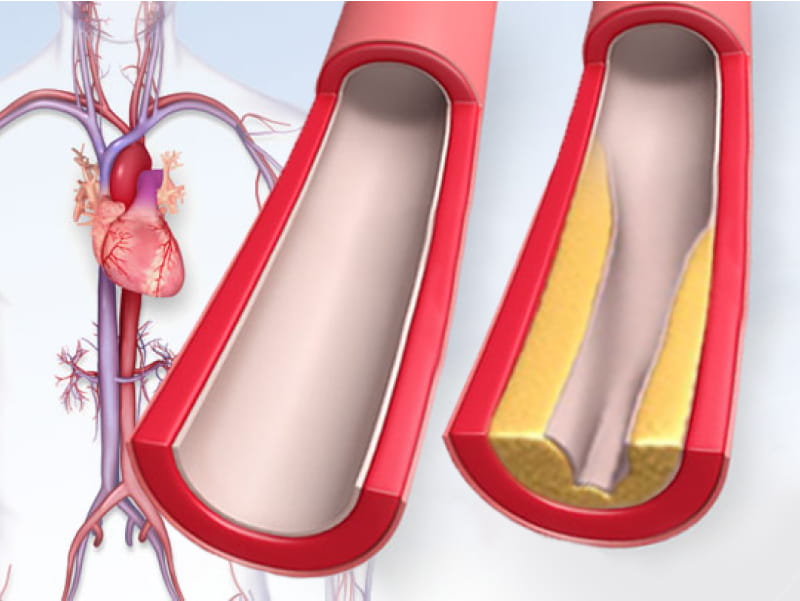
Cholesterol is carried in the blood in the form of high-density lipoproteins (HDL) and low-density lipoproteins (LDL). HDL cholesterol is “good” cholesterol. LDL cholesterol is the “bad” kind. A simple rule of thumb is that you want as little of the bad kind as possible.
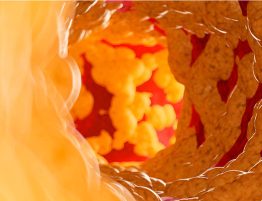
And that’s where treatment is emphasized. The bad kind of cholesterol can collect in the artery walls eventually causing stiffness and narrowing. This is atherosclerosis, which can be the basis of a heart attack or stroke.
Good cholesterol helps by removing the bad, although that’s not easy to do. HDL can only help in the fight, not win it.
“HDL is not something we try to alter with medication. It’s important in predicting risk but changing it is best done via lifestyle changes,” said Eckel, director of the Lipid Clinic at University of Colorado Hospital, and among the developers of the AHA’s Check. Change. Control. Cholesterol program to improve management of cholesterol. He also was part of the team that created the cholesterol guidelines that were published in 2013 and just updated in November 2018.
The total cholesterol figure you’ll get from your health care provider is based on HDL, LDL and a third factor: triglycerides. Triglycerides not only circulate in blood but are the most common type of fat in the body.
A high triglyceride level combined with high LDL or low HDL cholesterol is linked to those fatty buildups within the artery walls that increase the risk of heart attack and stroke.
What do cholesterol numbers mean?
Cholesterol numbers mean different things for each person’s situation.
Based on your personal risk, your cholesterol measures will be considered as you and your health care provider discuss what to do next.
“There are a lot of factors that enter into the determination of the best level for each individual. For instance, someone in their 40s and 50s the LDL cholesterol may be slightly elevated, but the person might have no other risk factors,” Eckel said.
Dr. Scott M. Grundy, chairman of the writing committee for the new cholesterol guidelines, notes that when doctors are working out an action plan with their patients, they should consider a person’s “risk-enhancing factors” such as family history, kidney disease or other personal scenarios.
“These are important,” said Grundy, a professor of internal medicine at the University of Texas Southwestern Medical Center and Veterans Affairs Medical Center in Dallas. “Patients should be aware of these and work to determine how to think about them with their doctor.”
How is elevated or high cholesterol treated?
Treatment comes in two forms: lifestyle changes and medication.
“We always want people to start with making lifestyle changes,” Eckel said. “That means eating a diet low in saturated fat and trans fats, and enriched with fruits and vegetables, whole grains, legumes, lean meat, fish and nuts. Another lifestyle change is being physically more active.”
If that sounds like a plan for losing excess weight and keeping it off, that’s exactly the point. A healthy body weight helps reduce LDL levels and helps people with normal cholesterol levels stay that way.
Sometimes, diet and exercise alone are enough to get numbers into the comfort zone. Sometimes, they’re not. For those people, the next option is usually taking a cholesterol-lowering medication called a statin.
“This is a very well-proven, evidence-based option,” Eckel said. “A lot of clinical trials strongly support taking statins.”
Again, your health care provider plays a key role, determining the type and dose that’s best for you. In some cases, your provider may prescribe other or additional medications that are not statins, such as ezetimibe or a PCSK9 inhibitor.
“The neat thing about cholesterol-lowering plans is that you can see changes quite quickly,” Eckel said, noting that cholesterol levels can improve within weeks of diet changes or medications.
Find more news from Scientific Sessions.
If you have questions or comments about this story, please email [email protected].